December 16, 2020
Hospitals are a unique environment for the spread of infectious diseases. COVID-19 aside, each year in the United States, healthcare-associated infections (HAIs) kill over 100,000 people annually. These healthcare-associated infections are considered errors in patient care and occur when a patient enters medical care for an ailment and becomes infected by a disease or virus unrelated to their original health issue. A comprehensive study completed by the Hospital Microbiome Project at the University of Chicago, Illinois, determined that healthcare-associated infections are most significantly caused by poor indoor air quality (IAQ).
The climate of Health care facilities has been changed forever due to the current COVID-19 pandemic. It is more important than ever for health care facility management to fully understand their buildings IAQ and the effects it will have on their occupants. The use of highly efficient particle filtration in centralized HVAC systems reduces the airborne load of infectious particles (Azimi and Stephens 2013). According to ASHRAE various strategies have been found to be effective at controlling transmission, including optimized airflow patterns, directional airflow, zone pressurization, dilution ventilation, in-room aircleaning systems, general exhaust ventilation, personalized ventilation, local exhaust ventilation at the source, central system filtration, UVGI, and controlling indoor temperature and relative humidity
Contact Sanitation is an Incomplete Pathogen Eradication Method
Healthcare-associated infections occur in what the study describes as an environment of biological extremes. An environment of biological extremes does not occur naturally. Counterintuitively, it can exist in areas of limited physical space where there is a heightened state of virulence from anti-microbial medications and housekeeping disinfectants attempting to eradicate pathogens.
Anti-microbial medications, sanitation equipment, and housekeeping disinfectants have historically been the common practice of hospital disinfectant programs, but in extreme cases, they can lead to stronger and more resistant pathogens that rapidly reproduce and thrive in the interior environment. There are often vulnerable patients inside hospitals with decreased immune defenses who are extremely susceptible to these pathogens.
Contact sanitation, which is the use of anti-microbial medications, sterilizers, and disinfectants, targets the transmission of pathogens through contact and short distance interruption of large droplets. This sanitation strategy, however, does not interrupt all the means that pathogens have to spread throughout an interior space.
Pathogens Can Spread Through the Interior Air
Pathogens can exist in droplet nuclei, which are aerosolized molecules less than five micrometers in diameter. Droplet nuclei can travel for extended periods through the air and are easily inhaled by patients or staff in a hospital.
Studies have shown that approximately 10 to 33 percent of all healthcare-associated infections travel through the air at some point between their initial source, the reservoir, and the eventual patient that they infect. Sanitation plans preventing pathogens spread through the air in medical facilities have historically not been as robust as contact sanitation plans.
Using Indoor Air Quality Management to Prevent Infections
The study conducted by the Hospital Microbiome Project at the University of Chicago suggests that hospitals could target infectious disease spread economically and effectively by actively managing their interior air quality.
As a result of the study, it was concluded that indoor relative humidity was the most statistically significant, independent variable affecting microbial spread throughout medical facilities. There was also a strong correlation detected between the presence of microbial communities and higher temperatures in rooms. The correlations between indoor air quality management and infectious disease spread are seasonal, and so air quality management becomes even more important during the winter months of a region.
Relative humidity was the key air quality determinant in the study. The relative humidity is the amount of water vapor present in air expressed as a percentage of the amount needed for saturation at the same temperature. Proper employment of heating, ventilation, and air conditioning systems in medical facilities is the essential way to manage indoor air quality and maintain proper relative humidity levels.
The study by the Hospital Microbiome Project at the University of Chicago determined that a relative humidity below 40 percent was associated with an increased prevalence of healthcare-associated infections. The study suggested that maintaining indoor relative humidity between 40-60 percent relative humidity may be an effective and cost-efficient method of decreasing the spread of pathogens inside facilities.
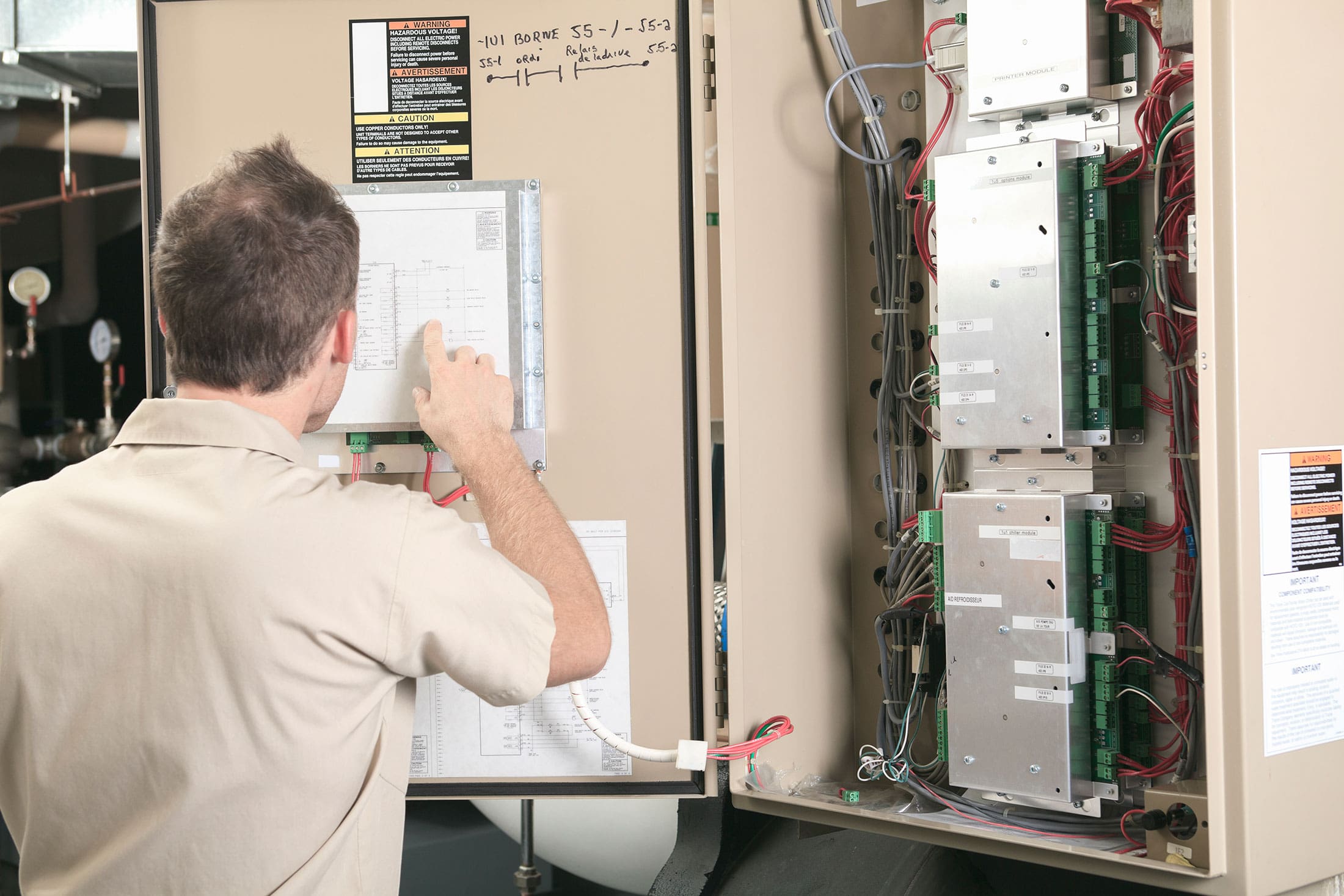
The Responsibility is on Hospital Engineers and Facility Managers
The study completed by the Hospital Microbiome Project at the University of Chicago provides hospital engineers and facility managers with better data to guide their building management. Facility managers should create comprehensive plans to both monitors and maintain the indoor air quality in patient’s rooms and hospital interior areas.
Maintaining relative humidity levels economically requires accurate monitoring capabilities and efficient HVAC systems in place to manage the large interior space inside hospitals. Hospitals often must invest in robust HVAC systems to meet the stringent demands of their air quality management plans. The best method of protecting these investments in HVAC equipment is to emplace comprehensive maintenance plans for the equipment.
Maintenance Opportunities To Reduce Risks
Keeping Cooling Towers Clean is an effective way to provide quality IAQ by reducing the risk that outdoor air isn’t infected. Cooling towers that supply water for central air-conditioning systems, in general, are a common culprit for outbreaks of disease. These cooling towers can add to risks by emitting infected water vapor, which can be brought inside through fresh air ventilation points, and general entrances like windows, doors, etc. The best maintenance practices to prevent both viral and bacterial contamination inside cooling towers are aggressive cleaning plans paired with personnel training, monitoring, and testing. Our CTV-1501 TowerVac® Cooling Tower Vacuum safely removes solids from boiling tower basins common areas for bacteria, like Legionella and other micro-organisms, to flourish.
Cleaning and decontaminating ductwork is also a effective method for maintaining a healthy building. When evidence of microbial growth in your HVAC system or ductwork is present consider chemical antimicrobial solutions specially designed for HVAC systems.
There are also experts available and willing to help facility managers review their current maintenance plans or to create new plans altogether. As demonstrated by the Hospital Microbiome Project, indoor air quality is one of the most important building conditions to manage the spread of healthcare-associated infections. Facility managers and hospital engineers owe it to their patients to take an active role in maintaining indoor air quality and provide the safest environment possible to their patients.

